Early Intervention Dosage Article
“Dosage” Decisions for Early Intervention Services
Authors:
Miriam Kuhn University of Nebraska at Omaha
Christine Marvin University of Nebraska-Lincoln
Reformatted from:
Kuhn, M., & Marvin, C. (2015). “Dosage” decisions for early intervention services. Young Exceptional Children. Advance online publication. doi: 1096250615576807
Scenario
Evan is 2 years old. He has been referred by his pediatrician to the early intervention program in his small town due to signs of global developmental delay. Evan says two words—ma (for mom, dad or grandma) and ba (for bottle.) He is still on a bottle and rejects many table foods. Evan began walking four months ago, and still falls down quite a bit. Although his parents report that Evan is generally a happy toddler, when he becomes upset he is prone to intense temper tantrums that include screaming and kicking. His parents handle these episodes in a calm, consistent manner and Evan typically regains his composure within two or three minutes. His mother and father teach in the local school district and Evan is cared for by his grandmother during the school day. Evan’s parents are quite engaged in seeking support for Evan; they vow to do everything in their power to promote his development.
Bryce is also 2 years old. He was referred to the early intervention program in the same small town by a caseworker with the Department of Health and Human Services (DHHS) as required by law under CAPTA (the Child Abuse Prevention and Treatment Act). Bryce was found one rainy day wandering alone outside the ground-level apartment where he lives with his mother and baby sister. He had succeeded in opening the screen door and walked out unnoticed. A passer-by spotted him and called the police. A DHHS caseworker was assigned to investigate the circumstances. During her visits, the caseworker observed that Bryce communicated by grunting and pointing to things, but she did not hear him using understandable words. Bryce’s mother reported that he was usually good-natured, but the caseworker noticed that when he became upset he was prone to intense temper tantrums that included screaming and kicking. Bryce’s mother did not seem to know what to do with him at that point, and she told the caseworker she usually gave him what he wanted because he “was so upset.” Bryce was not removed from his home because his mother voluntarily agreed to services offered by the caseworker. The caseworker also explained that she was required by the CAPTA provision to refer Bryce and his family to the early intervention program for assessment of Bryce’s development; Bryce’s mother expressed interest in the program.
The local community’s Early Intervention multidisciplinary team completed assessments of both children. The assessments included observations and standardized instruments completed with the boys and their parents to determine the children’s eligibility for services. While results of the observations and standardized assessments revealed that both Evan and Bryce qualified for early intervention services as children with developmental delays in cognitive and language development, many questions remained for their early intervention teams. What were the families’ priorities for their children? What supports would be optimal to effect positive outcomes for these children? What dosage of service from the early intervention team would be needed—how often and how intensive?
Part C of the Individuals with Disabilities Education Improvement Act (IDEA) of 2004 requires early intervention teams craft individualized and effective plans to meet the needs of young children with special needs and their families (Küpper, 2012). The newly updated Recommended Practices in Early Intervention/Early Childhood Special Education (Division of Early Childhood [DEC], 2014) reiterate the importance of promoting families’ active participation in making decisions regarding goals, supports, and the services needed for their children and themselves. Specifically, early interventionists are reminded of the importance of embracing a set of family-centered (F1, F3) and capacity-building practices (F5, F6) that lead to family-professional collaboration (F4, F7) aimed at developing an effective service plan to help families achieve their goals.
Many early intervention teams, however, may struggle to follow a process that results in systematically meeting the spirit of IDEA Part C or these recommended practices for families of children with special needs (McWilliam, 2010). This paper describes a process to help early intervention teams consider key factors in the design of a program’s focus and the type and intensity of supports appropriate for young children and their families. Relevant DEC Recommended Practices are noted as support for the questions the team should consider in this decision-making process. Decisions regarding Evan and Bryce are used to highlight how the interventions designed for these two boys compare when teams consider individualized needs of families and children.
Considerations for Optimal “Dosage” of Early Intervention Services
Generally, the concept of “dosage” is drawn from the fields of medicine and pharmacology wherein the term refers to amount and/or frequency of treatment. Early intervention services are not, however, tangible, easily quantifiable objects such as medicines. Educational scholars have advocated describing dosage parameters, such as the form, frequency, duration, and delivery mechanism of interventions, as a helpful means for accurately portraying the treatment intensity of educational interventions (Parker-McGowan et al., 2014; Warren, Fey, & Yoder, 2007). Bagnato, Suen, and Fevola (2011 ) proposed a definition of “dosage” in early intervention services as the “amount of time that an individual child must engage and participate in an early childhood intervention program or service to show measurable functional progress” (p. 119). This definition recognizes that “dosage” captures more than just number of hours or days of service provided. The essential learning activities that occur within and between those service contacts must happen with appropriate frequency, focus, and intensity for families and children, resulting in meaningful growth for the participants.
Historically, many decisions regarding the design and scheduling of early intervention were associated with identifying relevant learning experiences/activities for children and often influenced by the type or severity of young children’s disabilities, with more frequent and intensive learning activities provided to children with more significant challenges. Dunst (2012) points out, however, that after 1986 and the authorization of IDEA Part C, an unfortunate shift occurred in early intervention programming to a focus on type and frequency of professional services and less attention was given to the type and frequency of learning experiences that might benefit children and families. Furthermore, a focus on disability severity to decide the intervention plan has not had consistent support in the research literature (Behl, White, & Escobar, 1993; Ramey et al., 1992), as children with less severe disabilities have been shown to demonstrate the strongest outcomes from interventions (Palmer et al., 1988; Shonkoff, Hauser-Cram, Krauss, & Upshur, 1992). It can be argued however, that children with more significant challenges and their families also benefit from the expertise and support offered by early intervention programs. The fact that the payoff in terms of measureable outcomes for children with severe disabilities is smaller than for some children with milder disabilities is not a reason to reduce dosage of early intervention supports and services for children with severe disabilities. Finally, Shelden and Rush (2001) report that early intervention that supports early learning experiences in children’s homes with their usual caregivers yields significant improvements in developmental skills for many children with a range of abilities, environmental risk factors, and/or diagnoses. So a renewed focus on children’s needed experiences and supports, driven by consideration of families’ strengths and priorities for the children, as well as available professional expertise may more appropriately guide decisions about dosage of early intervention programs.
Early intervention teams should aim to encourage children’s care providers to weave into the fabric of their everyday lives rich, interesting, and engaging learning opportunities. Everyday experiences become development-instigating learning opportunities (Dunst et al., 2001) when they promote children’s exploration of their environments and practice toward competence. In addition to having stimulating home experiences, the responsiveness of caregivers can enhance children’s development, and contingent reinforcement of children’s social initiations often prompts their learning and generalization. It is not enough, therefore, for an early interventionist to just visit a home or visit frequently. Rather, optimization of natural learning environments and empowerment of caregivers as supports and first teachers of their children must occur. A multitude of potential opportunities for children’s learning occur between visits from the early interventionist.
Team members, charged with developing quality Individual Family Service Plans (IFSPs), must think deeply about the family characteristics that shape parents’ abilities to provide such learning environments for children with disabilities (Turnbull, Turnbull, Erwin, Soodak, & Shogren, 2011) as well as the configuration of resources offered by the early intervention program to support and assist the families and children (Shelden & Rush, 2010). Family characteristics can influence the targets and possibly the strategies used in early intervention while a well-designed set of program supports and services can be assembled to address the appropriate dosage of services for the desired targets. Teams need to consider (1) traits of the adult learners in the home, (2) social and cultural factors that influence effective early intervention practices, (3) what is needed to nurture parent-professional partnerships, and (4) how to best match the strengths of early intervention providers to the needs of individual families and children.
Adults as learners. Early interventionists whose aim is to improve the capacity of adult caregivers to provide support to children with disabilities must understand characteristics of adult learners. Adults learn best when they are actively engaged, when the context is highly interesting to them, when they receive information in multiple ways, when they can practice applying the new skill which has been taught, and when they have opportunities to self-assess through reflection (Friedman & Woods, 2012). Some adults will prefer, or may benefit from, more frequent contacts with the early interventionist because they want support in implementing a number of strategies or more complex interventions. Other adults may prefer, or benefit from, spacing between visits with an early interventionist to allow ample opportunities to implement the strategies they are confident in using with their children before discussing their efforts with the early interventionist.
The multidisciplinary team completed an interview with both Evan and Bryce’s families independently to collect information about, among many other things, the parents’ preferred learning styles. This information was invaluable in helping team members understand the best methods of providing developmental information for promoting Evan and Bryce’s cognitive and language development. For example, the team learned that Evan’s father enjoyed carpentry, and the early interventionist encouraged him when he described wanting to build Evan a toy barn. She then coached both of Evan’s parents in ways to prompt Evan’s play and simple requesting for help with the animals, blocks, and tractors in his new barn.
Social and cultural factors. Teams must also consider social and cultural factors that promote or hinder the delivery of effective early intervention services. Families in poverty typically benefit from regular, frequent visits, but Sharp, Ispa, Thornburg, and Lane (2003) found several factors compromised regular visiting rates in one such population of families who were participating in Early Head Start. Among these were mother’s age, high family mobility, emotional availability of the caretaker, cognitive skills of the parent, and the quality of the relationship with the home visitor. With or without issues of poverty, families with multiple risk factors, such as domestic violence, child maltreatment, substance abuse, teenage parents, or mental health concerns present additional hurdles to providing successful child and family supports, such as Part C early intervention (Azzi-Lessing, 2011; Yates, Obradović, & Egeland, 2010 ). Early intervention, though essential, will likely not be sufficient to address all the challenges facing these children and families. It is probable that a set of comprehensive, well-coordinated programs will be needed to address the multiplicity of needs (Schumacher, Hamm, Goldstein, & Lombardi, 2006).
The family interview with Bryce’s mother revealed a number of risk factors were posing challenges for this family. Bryce’s mother had not finished high school, but she was employed in a part-time job. She shared that she often lacked funds to meet her monthly budget for rent, utilities, and food for her family. She did report she had strong extended family support from her grandmother who often cared for the two children while she worked. Bryce’s mother expressed a fear that Bryce would have trouble learning because “school was hard” for her. The early intervention services coordinator and Bryce’s mother identified additional community partners offering supports Bryce’s mother wanted to pursue. These included an adult education program, a food pantry, and an energy assistance program. In addition, the caseworker from DHHS and Bryce’s great-grandmother had attended the assessment and pre-IFSP sessions with Bryce’s mother. At Bryce’s IFSP meeting, the team decided that both Bryce’s mother and great-grandmother would participate in the early intervention home visits to promote consistent use of strategies with him across the two environments where he spent most of his time.
Parent-professional partnerships. The development of successful partnerships between family members and early interventionists is essential for an effective dosage of early intervention to occur. Several important features of such collaborative relationships have emerged in the literature. Parents value early interventionists who are responsive, trustworthy, available, and empowering (Weatherston, 2010). Honest, but respectful communication is a key for developing trust in parent-professional relationships (Knoche, Kuhn, & Eum, 2013). Families appreciate strength-based, family-centered approaches to services (Dunst, Boyd, Trivette, & Hamby, 2002; Paulsell, Boller, Hallgren, & Esposito, 2010). DEC Recommended Practices (2014) define family-centered services as “practices that treat families with dignity and respect; are individualized, flexible, and responsive to each family’s unique circumstances; provide family members complete and unbiased information to make informed decisions; and involve family members in acting on choices to strengthen child, parent, and family functioning” (p. 9).
Studies have shown that the quality of relationships between family members and home visitors influences parents’ effectiveness in caring for children, the quality of family engagement in home visiting programs, as well as developmental outcomes for children (Paulsell et al., 2010; Knoche et al., 2012). Furthermore, the “parent’s level of engagement in intervention activities has been found to relate to…use of the strategies between home visits (Peterson, Luze, Eshbaugh, Jeon, & Kantz, 2007, p. 121). This utilization of strategies with children within children’s natural environments and daily routines provides the “dosage” of needed intervention that brings about meaningful, functional improvements for children.
Evan and Bryce’s IFSP teams were committed to providing family-centered early intervention services, thus, all early intervention providers received on-going professional development to enhance their skills for developing collaborative partnerships with families. When Evan was referred for an initial assessment by the multidisciplinary team, his parents were asked about their concerns for his development and they were engaged in the assessment by completing a developmental checklist and participating in a routines-based interview. These initial efforts to partner with Evan’s family laid a foundation of trust and mutual respect between his parents and the other team members. The assessment information allowed the team to generate functional outcomes for Evan that were priorities for his family, and in turn, prompted team discussion regarding effective interventions for achieving those outcomes.
Provider and program strengths. Early intervention teams are composed of individual professionals with varied backgrounds, experiences, strengths, and areas of interest. Members with greater skill and confidence may more efficiently effect changes than novice, less confident practitioners. Teams need to consider the unique skill sets each service provider possesses when planning supports for particular families.
In addition, there are a number of program variables that have been described in the literature as fundamental to early intervention’s mission of effectively supporting families to maximize the development of young children with disabilities. Programs that embrace capacity-building help-giving and family-systems interventions have been found to have direct effects on parent self-efficacy and well-being, which in turn have indirect effects on parent-child interactions and child development outcomes (Trivette, Dunst, & Hamby, 2010). Efforts should be made to maximize the percentage of time within home visits that is devoted to supporting dyadic, parent-child interactions (McCollum & Yates, 1994). Parent-child engagement has a powerful effect on child outcomes, but researchers have found that early interventionists do not spend as much time on it as they think they do (Basu, Salisbury, & Thorkildsen, 2010; Peterson et al., 2007). Finally, programs emphasizing a strong assessment system yield positive outcomes for children. Effective assessment occurs when programs have systems in place to demonstrate planning for learning opportunities, document the practice of parent- and provider-developed strategies, and collect data that would inform decision-making (Bernheimer & Keough, 1995; Sheridan, Clarke, Knoche, & Edwards, 2006). Such systematic procedures for delivering support and collecting data about the effectiveness of the supports enhance the ability of IFSP teams to determine whether or not the “dosage” of service provided is appropriate.
The early interventionist providing services for Bryce worked strategically with his mother to identify learning opportunities for addressing priority outcomes identified in the IFSP. Together, they devised a calendar system so that Bryce’s mother would have a visual reminder of the routines and daily activities in which she could prompt and he could practice two targeted skills, one promoting his communication and another his cognitive abilities. Bryce’s mother then came up with the idea of putting on the calendar a ranking between 1 and 5 to indicate how well Bryce had done on each of the targeted behaviors that day. When the early interventionist visited Bryce’s home she was able to see on the family calendar how the week had gone and coach Bryce’s mother for modifications to the plan in terms of adjusting goals and/or teaching strategies for Bryce.
A Decision-Making Process for Determining “Dosage” of Early Intervention Services
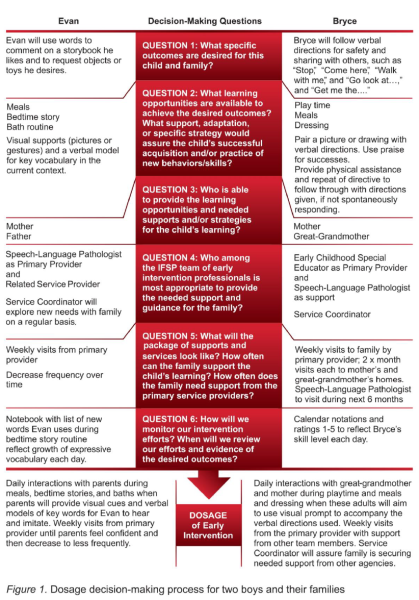
Families who have children who qualify for early intervention demonstrate distinctive constellations of child and family characteristics, and the programs which aim to support them bring their own set of unique resources in the expertise of the service providers. It is no wonder IFSP teams struggle to determine how best to support individual families and children. The use of a decision-making process, such as the one shown in Figure 1, would allow teams to make individualized decisions about what a particular child and family need in terms of supports and services, keeping in mind the salient characteristics of that child and family and the optimal array of resources offered by an early intervention program that grounds its efforts in recommended practices for early intervention (DEC, 2014). Teams could work through this process by answering the following series of questions as they discuss the IFSP design with families. Specific DEC Recommended Practices are noted by identifying letter and number in parentheses.
(From: Young Exceptional Children DOI: 10.1177/1096250615576807)
Question 1. What specific outcomes are desired for this child and family?
Outcomes should be stated in functional, measureable terms that allow teams to have a clear vision of when goals will be considered as accomplishments. This presumes that the team has utilized a thorough assessment process to gather information about unique child and family strengths and challenges, as well as become knowledgeable about a family’s desired outcomes for their child with the disability (DEC Recommended Practices: INS3). For example, although both Evan and Bryce showed delays in language development, their targeted communication goals were not identical, reflecting input and priorities of the individual families.
Question 2. What learning opportunities and strategies are needed to achieve the desired outcomes?
First, the team should identify the natural learning environments where the outcomes might be prompted, demonstrated, and observed. The team might explore what existing daily routines and activities are/will be available to provide numerous opportunities for the child to develop, use, and refine targeted behaviors/skills in meaningful, authentic ways (INS5). Secondly, what support, adaptation, or specific strategy would assure the child’s successful acquisition and/or practice of new behaviors/skills (INS4)? Potential interventions may include accommodations for children’s specific needs in daily activities, modifications of materials, routines, environments, and/or adult-child interaction strategies designed to prompt and/or reinforce specific skills. At this stage in the process, Evan’s and Bryce’s teams begin to conceptualize an intervention plan needed to attain the desired outcomes for the individual children and families.
Question 3. Who is able to provide the learning opportunities and needed supports and/or strategies for the child’s learning?
Persons available to support young children’s learning include the parents, older siblings, grandparents, or child-care providers who interact with the children on a daily basis. Teams should aim to support and enhance these family-child relationships in ways that build on family strengths and capacities (F5). Some parents, like Evan’s, may feel comfortable and confident that they are able to proceed with accommodations/supports for their child with limited assistance from other family members or members of the early intervention team. Other families, like Bryce’s, are desirous of support for multiple care providers and partnering with early intervention professionals more intensively to access expertise and support needed to implement the demonstrated/suggested intervention strategies more effectively.
Question 4. Who among the IFSP team of early intervention professionals is most appropriate to provide the needed support and guidance for the family?
If the family chooses to access support from the early intervention team, then a team member with the needed expertise and availability would become the primary service provider for the family (TC5). The team should consider the desired outcomes and the interventions planned, and also determine whether the primary service provider or family will need support from additional early intervention team members. Within this system, the team, represented by a variety of early intervention professionals, is available to regularly meet with and coach the primary service provider in his/her efforts to support a family, and/or accompany the primary service provider on co-visits with the family (Shelden & Rush, 2010; TC3). For example, the primary service provider for Evan and his family was the speech-language pathologist, while the early childhood special educator was deemed to be the most appropriate primary service provider for Bryce and his family.
Question 5. What will the package of supports and services look like? How often can the family support the child’s learning? How often does the family need support from the primary service provider?
The team should determine the sorts of support preferred and needed by the family to enhance their “competence and confidence in using natural learning opportunities to foster their child’s learning and development” (Shelden & Rush, 2010, p. 189; F5, F6, INS10). The team should discuss with the family a plan that provides the array of supports—for the family, for the child, and for the primary service provider— that can optimize the achievement of targeted IFSP outcomes in a reasonable time period. At this stage in the process, the team should aim to solidify decisions about frequency, intensity, and duration of supports and services.
Characteristics of chosen interventions may influence frequency of home visits needed for successful implementation. Teams should consider the newness of the intervention for the family and provider, how complex it is to implement, and how comfortable the family is with implementation. Next, consider whether or not the intervention will promote rapid skill development (necessitating less time between visits), or take some time and patience to have an effect. Finally, teams should take note of the family’s learning style. Some families will ask for more concrete or specific support, while others prefer more freedom to shape their own learning.
When supporting families’ use of interventions, Keilty (2010) cautions that there are dangers both in scheduling home visits too infrequently or too frequently. The problems with visits occurring too infrequently are that families may need more guidance in applying strategies or may need more options to try, or they may have questions about interventions which go too long unanswered. In these cases, children are not receiving frequent opportunities to learn and practice new skills throughout their daily routines. On the other hand, if visits occur too frequently, families may begin to lack confidence in their abilities to utilize interventions when the professional is not there, become dependent on the home visitor as the change agent, or may not have enough chances to give an intervention a good try before the subsequent home visit. At this stage, the team decision-making process requires maximum flexibility in documenting frequency and intensity statements in the IFSP to match the team’s vision for delivering support with enough frequency that families feel supported in using planned approaches to help their children achieve desired outcomes (Keilty, 2010).
Question 6. How will we monitor our intervention efforts? When will we review our efforts and evidence of the desired outcomes?
Effective teams make specific plans to monitor the effects of their interventions so that strategies may be continued or modified as needed to meet designated benchmarks (A9). Collecting and analyzing data to inform such decisions may prove challenging for early interventionists and downright foreign for parents who have little experience with these practices. Nevertheless, this is a critical step in understanding if the correct type and dosage of intervention is in place. Brawley and Stormont (2014) suggested blending qualitative and quantitative methods of collecting data to reach more credible conclusions regarding children’s progress, as well as using visual displays of data to prompt family-team discussions, analyses, and decision-making. Such practices allow teams to make appropriate decisions about continuing a strategy or modifying it. This also promotes a cycle of decision-making by aiding teams in identifying the next desired target of intervention or need for different professional expertise, or knowing when to celebrate accomplishments and discontinue services. Figure 1 describes the distinct progress monitoring decisions made by Evan’s and Bryce’s teams.
Conclusion
Through this decision-making process, a set of clear outcomes for the child and family are defined. Furthermore, the primary service provider and family develop a shared vision of what supports are needed and how often they will need to meet. The family understands the vital role they will play every day in their child’s development. All team members are prepared to support the process efficiently and effectively, and data is collected and analyzed to monitor the child’s progress given the plan of support. Teams following this process will form dosage decisions based on families’ contexts, strengths, and priorities for their children. The dosage of early intervention supports will reflect the coaching needs of families and primary providers that promote children’s participation in family life. Such a process allows early intervention teams to meet both the letter of Part C legislation, as well as the spirit of the law, and in doing so, engage in recommended practices when supporting diverse populations of families and children with special needs.
Evan and Bryce Re-Visited
Evan. Evan’s IFSP team defined specific improvements in Evan’s cognitive understanding of concepts and use of expressive language as their priority desired outcomes. One goal developed by the team was: Evan will use words to comment on a storybook he likes and to request objects (food or toys) he desires. To address this goal the team identified learning opportunities in Evan’s meal time, bath, and bedtime story routines and identified his mother and father as key adults to use visual supports paired with verbal models during these routines to encourage Evan’s use of words. Evan’s parents requested support from an early interventionist so they could learn the intervention strategies, develop the visual materials needed, and receive feedback from the primary service provider on their use of the strategy with Evan. The team determined the speech-language pathologist had expertise needed for this intervention plan and would meet with Evan’s family regularly as the primary service provider. The team further decided that additional related service providers’ expertise and support were not needed at that time. The family asked the service coordinator to check back with them on a periodic basis in case any needs for community support arose, although none were identified at the initial IFSP meeting. The package of services for Evan and his family became clear. To begin, weekly visits to Evan’s home were appropriate to enable the speech-language pathologist and Evan’s parents to establish the strategies that would be used to promote his comprehension of concepts and use of expressive language during meal, bath, and bedtime story routines. Evan’s parents felt that once the intervention was in place, they would need to see the service provider less frequently in order to have adequate time to implement the plan discussed at the previous meeting. The speech-language pathologist partnered with Evan’s parents to devise a method of documentation regarding his progress toward the functional goal of using words to comment within his daily routines. Evan’s mother wanted to record all the new words she heard him imitate or say spontaneously during the bedtime story reading routine in a small notebook. The speech-language pathologist would review this list with Evan’s parents at the beginning of each home visit, and the data would drive future decisions about interventions and frequency of home visits.
Bryce. Bryce’s IFSP team defined specific improvements in Bryce’s understanding of language and following of directions as priority desired outcomes. One goal developed by the team was: Bryce will follow verbal directions for safety and sharing with others, such as “Stop,” “Come here,” “Walk with me,” and, “Go look at...,” and “Get me the….” To address this goal, the team identified learning opportunities in Bryce’s play times, meals, and dressing routines at home and his great-grandmother’s home. Bryce’s mother and great-grandmother were identified as key adults to use a set of behavioral strategies to assist Bryce with understanding and following directions that included consistently pairing a visual prompt with the verbal direction, praising Bryce for following the direction independently, and providing immediate physical assistance to follow the direction if he did not comply independently. Bryce’s mother requested visits occur at her home and her grandmother’s home on alternate weeks so that both women would have support related to their use of the strategies. The team determined the early childhood special educator had expertise needed for this intervention plan and could meet with Bryce’s family regularly, so she was designated as the primary service provider. The team further decided that the speech-language pathologist’s expertise and support would be valuable and made available to the primary provider. Service coordination was included as a service on Bryce’s IFSP and several community agencies were listed as family supports. The package of services for Bryce and his family became clear. To begin, the educator, as primary service provider, would meet weekly with Bryce’s family—one week at Bryce’s home and the alternate week at his great-grandmother’s home. This would enable the primary provider to support Bryce’s mother and great-grandmother to establish the strategies that would be used to promote his receptive language and ability to follow directions during play times, meals, and dressing routines. The primary provider partnered with Bryce’s mother to devise the calendar system she desired to easily document his progress toward these functional outcomes, and the data collected in this manner would drive future decisions about interventions and frequency of visits. These data and questions from either family member would be shared with the speech-language pathologist on an as-needed basis and the speech-language pathologist might make a co-visit with the primary provider during the next three months to offer her expertise in assessing Bryce’s progress and need for changes in planned strategies or supports. The services coordinator would visit with Bryce’s mother weekly for the first month to establish steps needed to successfully access community resources and supports. Service coordinator visits would fade to one time monthly once those targeted resources and supports for the family were in place.
References
Azzi-Lessing, L. (2011). Home visitation programs: Critical issues and future directions. Early Childhood Research Quarterly, 26, 387-398.
Bagnato, S., Suen, H., & Fevola, A. (2011). “Dosage” effects on developmental progress during early childhood intervention: Accessible metrics for real-life research and advocacy. Infants and Young Children, 24(2), 117-132.
Basu, S., Salisbury, C., & Thorkildsen, T. (2010). Measuring collaborative consultation practices in natural environments. Journal of Early Intervention, 32(2), 127-150.
Behl, D., White, K., & Escobar, C. (1993). New Orleans early intervention study of children with visual impairments. Early Education and Development, 4, 256-274.
Bernheimer, L., & Keogh, B. (1995). Weaving interventions into the fabric of everyday life: An approach to family assessment. Topics in Early Childhood Special Education, 15, 415–433.
Brawley, S., & Stormont, M. (2014). Investigating reported data practices in early childhood: An exploratory study. Journal of Positive Behavior Interventions, 16 (2), 102-111.
Division for Early Childhood. (2014). DEC recommended practices in early intervention/early childhood special education 2014. Retrieved from http://www.dec-sped.org/recommendedpractices
Dunst, C. (2012). Parapatric speciation in the evolution of early intervention for infants and toddlers with disabilities and their families. Topics in Early Childhood Special Education, 31(4), 208-215.
Dunst, C. J., Boyd, K., Trivette, C. M., & Hamby, D. W. (2002). Family‐oriented program models and professional help giving practices. Family Relations, 51(3), 221-229.
Dunst, C., Bruder, M. B., Trivette, C., Hamby, D., Raab, M., & McLean, M. (2001). Characteristics and consequences of everyday natural learning opportunities. Topics in Early Childhood Special Education, 21(2), 68-92.
Friedman, M., & Woods, J. (2012). Caregiver coaching strategies for early intervention providers: Moving toward operational definitions. Infants and Young Children, 25(1), 62 -82.
Keilty, B. (2010). The early intervention guidebook for families and professionals: Partnering for success. New York, NY: Teacher's College Press.
Knoche, L., Sheridan, S., Clarke, B., Edwards, C., Marvin, C., Cline, K., & Kupzyk, K. (2012). Getting Ready: Results of a randomized trial of a relationship-focused intervention on the parent-infant relationship in rural Early Head Start. Infant Mental Health Journal, 33(5), 439-458. doi:10.1002/imhj.21320
Knoche, L. L., Kuhn, M., & Eum, J. (2013). " More time. More showing. More helping. That's how it sticks": The perspectives of early childhood coachees. Infants & Young Children, 26(4), 349-365.
Küpper, L. (Ed.). (2012, October). The basics of early intervention (Module 1). Building the legacy for our youngest children with disabilities: A training curriculum on Part C of IDEA 2004. Washington, DC: National Dissemination Center for Children with Disabilities.
McCollum, J., & Yates, T. (1994). Dyad as focus, triad as means: A family-centered approach to supporting parent-child interactions. Infants and Young Children, 6(4), 54-63.
McWilliam, R. (2010). Routines-based early intervention: Supporting young children and their families. Baltimore, MD: Paul H. Brookes.
Palmer, F., Shapiro, B., Wachtel, R., Allen, M., Hiller, J., Harryman, S., Mosher, B., Meinert, C., & Capute, A. (1988). The effects of physical therapy on cerebral palsy. New England Journal of Medicine, 318, 803-808.
Parker-McGowan, Q., Chen, M., Reichle, J., Pandit, S., Johnson, L, & Kreibich, S. (2014). Describing treatment intensity in milieu teaching interventions for children with developmental disabilities: A review. Langauge, Speech, and Hearing Services in Schools. Advance online publication. Retrieved from http://lshss.pubs.asha.org/
Paulsell, D., Boller, K., Hallgren, K., & Esposito, A. (2010). Assessing home visit quality: Dosage, content, and relationships. Zero to Three, 30(6), 16-21.
Peterson, C., Luze, G., Eshbaugh, E., Jeon, H.-J., & Ross Kantz, K. (2007). Enhancing parent-child interactions through home visiting: Promising practice or unfulfilled promise? Journal of Early Intervention, 29(2), 119-140.
Ramey, C., Bryant, D., Wasik, B., Sparling, J., Fendt, K., & LaVange, L. (1992). Infant health and development program for low birth weight, premature infants: Program elements, family participation, and child intelligence. Pediatrics, 89, 454-465.
Schumacher, R., Hamm, K., Goldstein, A., & Lombardi, J. (2006). Starting off right: Promoting early child development from birth in state early care and education initiatives. Retrieved from http://www.clasp.org/results?cx=002815250263393764720%3Af6r5qoodvty&cof=FORID%3A11&ie=UTF8&q=Promoting+early+child+development+from+birth+in+state+early+care+and+education+initiatives&sa=SEARCH
Sharp, E., Ispa, J., Thornburg, K., & Lane, V. (2003). Relations among mother and home visitor: Personality, relationship quality, and amount of time spent in home visits. Journal of Community Psychology, 31(6), 591-606.
Shelden, M., & Rush, D. (2001). The ten myths about providing early intervention services in natural environments. Infants and Young Children, 14(1), 1-13.
Shelden, M., & Rush, D. (2010). A primary-coach approach to teaming and supporting families in early childhood intervention. In R. McWilliam (Ed.), Working with families of young children with special needs (pp. 175–202). New York, NY: Guilford Press.
Sheridan, S., Clarke, B., Knoche, L., & Edwards, C. (2006). The effects of conjoint behavioral consultation in early childhood settings. Early Education and Development, 17(4), 593-617.
Shonkoff, J., Hauser-Cram, P., Krauss, M., & Upshur, C. (1992). Development of infants with disabilities and their families: Implications for theory and service delivery. Monographs of the Society for Research in Child Development, 57(6, Serial No. 230).
Trivette, C., Dunst, C., & Hamby, D. (2010). Influences of family-systems intervention practices on parent-child interactions and child development. Topics in Early Childhood Special Education, 30(1), 3-19.
Turnbull, A., Turnbull, R.. Erwin, E., Soodak, L., & Shogren, K. (2011). Families, professionals, and exceptionality: Positive outcomes through partnerships and trust. Boston, MA: Pearson.
Warren, S., Fey, M., & Yoder, P. (2007). Differential treatment intensity research: A missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews, 13, 70-77.
Weatherston, D. (2010). Infant mental health home visiting strategies: From the parents’ points of view. Zero to Three, 30(6), 52-57.
Yates, T., Obradović, J., & Egeland, B. (2010). Transactional relations across contextual strain, parenting quality and early childhood regulation and adaptation in a high-risk sample. Development and Psychopathology, 22(3), 539 - 555.
About the Authors:
Dr. Miriam Kuhn is an assistant professor in the Department of Special Education and Communication Disorders at the University of Nebraska at Omaha. She may be reached at miriamkuhn@unomaha.edu.
Dr. Christine A. Marvin is a professor in the Department of Special Education and Communication Disorders at the University of Nebraska- Lincoln. She may be reached at cmarvin1@unl.edu.